What Is PIN?
PIN is an abbreviation for Posterior Interosseous Nerve. It’s an extension of the radial nerve located in the forearm and supplies nerve stimulus to many of the muscles in the forearm. When it becomes entrapped, it can cause something called posterior interosseous syndrome.
What Is PIN Compression Syndrome?
PIN compression syndrome occurs when the nerve becomes entrapped in the area of the supinator muscle. The syndrome causes pain and negatively impacts the function of the elbow, hand and wrist.
What are the Symptoms of PIN Compression Syndrome?
The symptoms of PIN compression vary from patient to patient, depending on the severity of the compression. Most commonly, people complain of:
- Weakness and numbness in the arms and hands
- Weakness straightening the wrist
- Problem elevating fingers
- Fingers drop spontaneously
What Causes PIN Compression Syndrome?
PIN compression can occur for a number of reasons. It can occur spontaneously or develop over time. Causes include:
- Blunt trauma (a heavy blow sustained at work, during contact sports, or an accident)
- Repetitive movements
- Fracture
- Inflammation
- Tumours or cysts
- Penetrating trauma (a laceration at the forearm or a stab wound)
When Should I Consult a Doctor?
PIN compression syndrome can quickly go from bad to worse. If you are concerned about pain or mobility issues you are experiencing, it’s wise to contact your doctor as quickly as possible. Early diagnosis of this treatment can help patients achieve an acceptable outcome.
How Is PIN Compression Syndrome Diagnosed?
The first step is a thorough clinical examination. Your doctor will discuss your medical history and lifestyle. In addition, you may be asked to undergo:
- Electromyogram (EMG) to measure electrical activity in the muscles and identify whether nerve damage has occurred
- Nerve Conduction Study to assess the severity of the problem and to ensure the nerve is relaying signals effectively
- Imaging Tests – including X-ray, MRI or ultrasound
How is PIN Nerve Compression Treated?
At the time of diagnosis and depending on the severity of the symptoms, your doctor may suggest:
- Rest
- Physiotherapy
- Pain medication
- Corticosteroids
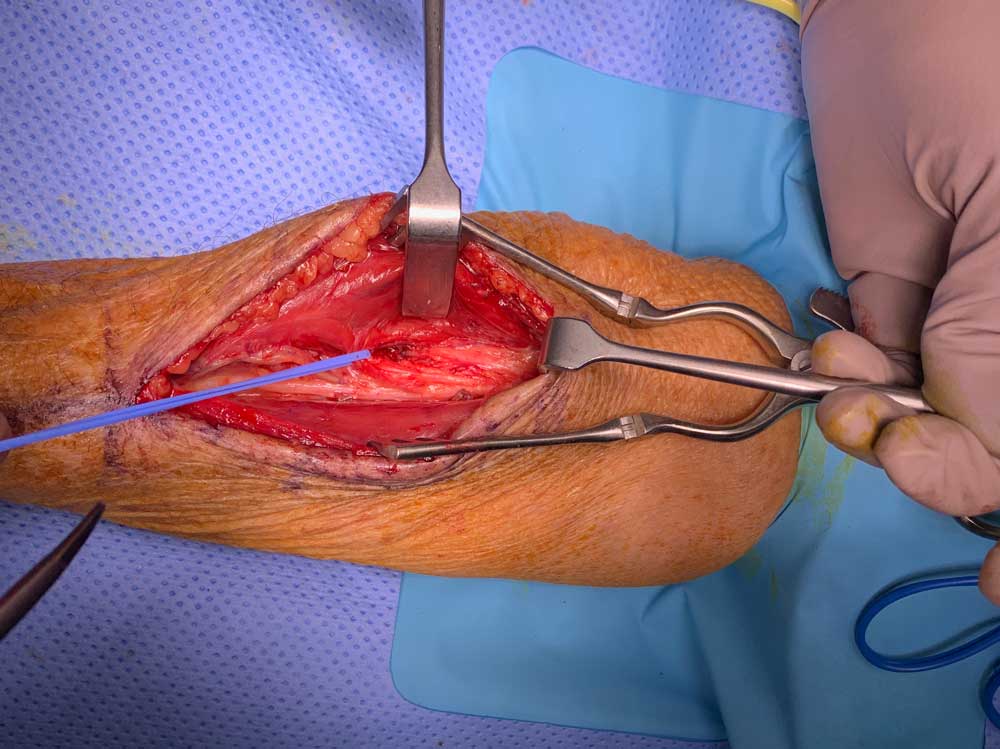
Nerve decompression surgery may be required to free the impacted nerve. In this procedure, the surgeon makes a small incision near the point of compression. The nerve is accessed, freed from pressure, and any fragments of bone or tissue contributing to the problem may be removed. Typically, surgery is performed under general anaesthesia.
What Can I Expect After PIN Decompression Surgery?
When your surgery is complete, you will be taken to a recovery room for observation. You will likely feel drowsy when you wake up. You can also expect:
- Pain around the surgical site which can be treated
What Should I Do After Surgery?
What you do after surgery is almost as important as what your doctor does during surgery. You will be given a set of post-surgical guidelines to help you help yourself heal successfully and maximise the benefits of your surgery.
Among the activities you will be asked to do:
- Take appropriate pain medication
- Elevate your arm above chest height as much as possible for the first day
- Wear a bandage
- Begin physical therapy
Most patients resume one-handed work activities by the 2nd week, followed by light duties including clerical work at 6-8 weeks. Heavy manual labour should not be resumed for 12 -16 weeks.
If pain and swelling increase and/or other symptoms of nerve compression return, consult Dr Sammons immediately.
Should I Follow Up with Dr Sammons after Surgery?
Yes. It’s important for Dr Sammons and your GP to monitor your progress. A practice nurse will contact you to schedule a follow-up visit a week after surgery. If any questions arise for you prior to your visit, do not hesitate to contact Dr Sammons. She is happy to talk things over and address any concerns you may have.
Is PIN Decompression Surgery a Permanent Solution?
The level of relief experienced by those who undergo nerve decompression procedure varies widely, from 10% to 95% (Source: National Institutes of Health). Residual symptoms are common, depending on the cause of the problem and the severity of symptoms prior to surgery.
Please call our rooms if you have any additional concerns or questions.